Billing & Financial Assistance Resources
Billing & Collections
Admission
Before the patient is admitted to the Hospital, the Admission’s team will make reasonable efforts to collect a patient’s insurance and other information and to verify coverage for the services to be provided. This information should be obtained prior to the delivery of non- emergent healthcare services.
After the Admission team receives a referral, they will verify insurance and check benefits. We will be reviewing to ensure insurance coverage is active and whether a plan is in-network or out-of-network. To assist with the accuracy of the insurance verification, please provide a copy of the patient’s insurance card(s), exact patient name, and date of birth.
- Each plan can vary on the level of coverage for inpatient rehabilitation including potential non-coverage for plans that are out-of-network.
- After benefits are verified, the Hospital Admission team will determine if an insurance authorization is required. If one is required, the Admissions team will start the authorization process for inpatient rehabilitation. This may take several days to receive a response from the insurance plan.
During and After the Patient’s Hospital Stay
After an admission is approved, the patient will admit and sign applicable Admission forms. During a patient’s stay, charges will be collected each day that include room and board, therapy, supplies, medications, labs, and other ancillary services performed.
After the patient is discharged from the hospital, all charges are summarized by service package and type of service. These summarized charges are billed to the applicable third-party payer.
The Central Business Office will bill all payers in accordance with contractual agreements and any applicable laws. After insurance payments have been settled and reflected on a patient’s account, the patient will receive statements from the Hospital requesting payment on the patient balance. Patients may be required to pay non-emergent healthcare services in advance for services that will not be covered by third-party payers, including co-payments, deductibles, and co-insurance amounts.
Collections and Eligibility for Financial Assistance
Once a patient has been discharged and the patient’s balance has been determined, the Central Business Office will initiate the patient statement series mailed each month in an attempt to collect the outstanding balances.
Collections on patient balances will be pursued for a minimum of 120 days before any collection agencies will be engaged. Billing statements will include a notice regarding the Financial Assistance Policy, including information on how to obtain copies of the Financial Assistance Policy and a Financial Assistance Application.
The Central Business Office will evaluate the Financial Assistance requests received to determine applicable discounts that can be applied to the patient’s balances.
- The Central Business Office will consider a patient’s total resources which would include, but are not limited to, an analysis of income and expenses. This would be done by having the patient complete a Financial Assessment Form and supply the necessary supporting documentation to make a determination of financial hardship.
- The Central Business Office must determine that no source other than the patient would be legally responsible for the patient’s medical bill.
- The patient’s file must contain documentation of the method by which indigence and hardship was determined including all the backup information substantiating the determination.
In addition, the Central Business Office will evaluate and potentially approve payment plans for patients who have difficulty paying their full account balance at one time. These are evaluated on a case-by-case basis. If no payment arrangements have been made and the Central Business Office collection efforts have been exhausted, the account can then be sent to a collection agency.
Financial Assistance Policy
ClearSky Health has a Financial Assistance and Charity Care policy to assist individuals who may be un-insured or under-insured and would meet the medical necessity guidelines for an inpatient rehabilitation stay at our hospital.
ClearSky Health will file all applicable insurance, Medicare, Medicaid, and other Third-Party Liability claims. If you qualify for any State or Local Funded Programs, please provide information regarding your application status. The financial assistance will apply to the patient balance after all insurances have been settled or to the private pay balance after the private pay discount.
To apply for Financial Assistance, you may request an application when you are being evaluated by our clinical staff before admission. You may also print off the application from this link.
Once you have completed and signed the application, it should be turned into our staff per instructions. This should be completed before your admission to the hospital; it is not a guarantee that your application will be approved.
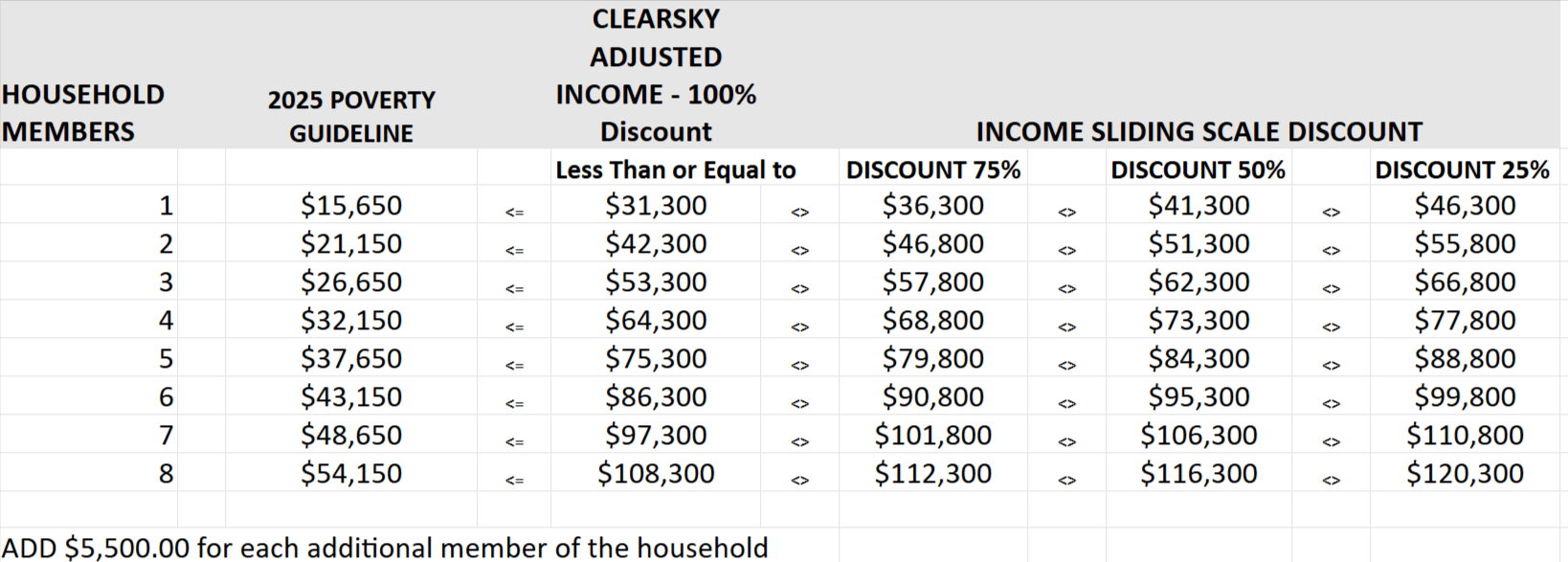
The application will be reviewed by our Central Business Office and will be either approved or denied based on the National Poverty Guidelines. The decision is based on the number of people in your household and the combined gross income of everyone in the household. Your portion of the patient’s responsibility may be partially or fully discounted based on the guideline. Patients whose family income is equal to or less than 200% of the Federal Poverty Guideline are generally eligible for free care. Patients whose income is above 200% of the Federal Poverty Guidelines may be eligible for a sliding scale discount. The Central Business Office will have a decision made and communicated to you after the application has been received by them.
This assistance does not apply to provider or physician fees. Please contact your practitioner directly to discuss their specific financial hardship processes. View Physician Listings Page.
For questions regarding the financial assistance, you may contact the Central Business Office by email or by calling us at 505-317-3956.
Financial Assistance Discount Guidelines
Financial Hardship Application
A Financial Hardship Application must be completed to determine if you will qualify for financial assistance and charity care. The Financial Hardship Application must be filled out completely and all supporting documentation attached before a determination can be made regarding final financial status. Click Here to View/Download Application.
The Financial Hardship Application will be reviewed to determine the level of assistance that can be provided. This determination may help with all or a percentage of the patient balance if approved.
ClearSky Health will file all insurance, Medicare, Medicaid and other Third-Party Liability claims. If you qualify for any State or Local Funded Programs, please provide information regarding your application status. The Charity Care request form is used as a last resource.
The Financial Hardship Application will only be in effect for the dates of service that are currently being rendered. (Does not cover indefinitely).
Financial Hardship Application Assistance
INSTRUCTIONS ON COMPLETING APPLICATION
Please complete the application and attach supporting documentation.
Application must be signed and dated by the patient requesting financial assistance.
- Patient information: print patient name and fill out the address, responsibly party and how long at the address at the top of the form. Please include the number of people that live in the household, including children and other dependents.
- Banking Information, Savings & Investment/Other Account Balance: List the total balances for checking, savings, or other investment accounts for all individuals in the household. Please include 401s, and other pension accounts.
- Income: Include the income of everyone in the household. Please list the gross amount of each individual in the household. This does include Social Security Income, retirement income, child support and any other type of income that is received by anyone in the household.
- Monthly Obligations: This portion of the application should include all expenses of the household and should only include the monthly payment amount that you pay for each outstanding expense that you have incurred.
- Application must be signed and dated by the patient requesting charity care.
- Submit the application to the Finance Department. The Finance Department will review the application and use the Federal Poverty Guidelines to determine if the patient qualifies for any discount. This is based on the income and total number of people in the household.
- Please scan and email all documents to Central Business Office email:
bu************@cl************.com
OR - Mail a copy of the completed application and all documents to:
ClearSky Health
ATTN: Business Office
5600 Wyoming Blvd. NE Suite 225
Albuquerque, NM 87109 - If you need additional assistance with the application, please call the Central Business Office at 505-317-3956.
How to Request an Itemized Statement
An itemized statement or bill may be requested and will be provided within 7 business days after the request or the discharge date, whichever is later. The itemized bill or statement will contain details of the individual charges by date. Physician services will not be included in this bill. You should contact the physician who provided the service to obtain an itemized bill or statement for the service provided.
Questions or concerns regarding your bill can be addressed by sending us an email to the email below or calling the number below:
- Central Business Office phone number: 505-317-3956
- Central Business Office email:
bu************@cl************.com
If you are not fully satisfied with the resolution to your questions or concerns, you may contact the Florida Agency for Health Care Administration directly at 888-419-3456 or 800-955-8771.
Physician & Provider Contact Information
Provided are the applicable names, mailing addresses, and telephone numbers of the health care practitioners and medical practice groups with which we contracted to provide services in our rehabilitation hospital. Please reach out to the providers for the below questions:
- To request a current physician or provider itemized statement
- To request a personalized estimate of reasonably anticipated practitioner or group charges for your specific condition.
- To contact the practitioners or groups to determine which health insurers and health maintenance organizations they participate in as network providers or preferred providers.
This listing is updated quarterly. Practitioners may be added or removed during this time. For questions or concerns, please call the hospital directly and ask to speak with Credentialing, so that we can assist you with the most current information.